In the realm of bariatric surgery, the gastric sleeve procedure has emerged as a transformative option for individuals seeking sustainable weight loss and improved health. Over the years, this surgical technique has undergone significant evolution, marked by advancements and innovations that have enhanced its efficacy and safety. From its humble beginnings to its current state-of-the-art applications, the journey of the هزینه عمل اسلیو معده جدید reflects the relentless pursuit of excellence in the field of obesity treatment.
The Genesis of Gastric Sleeve
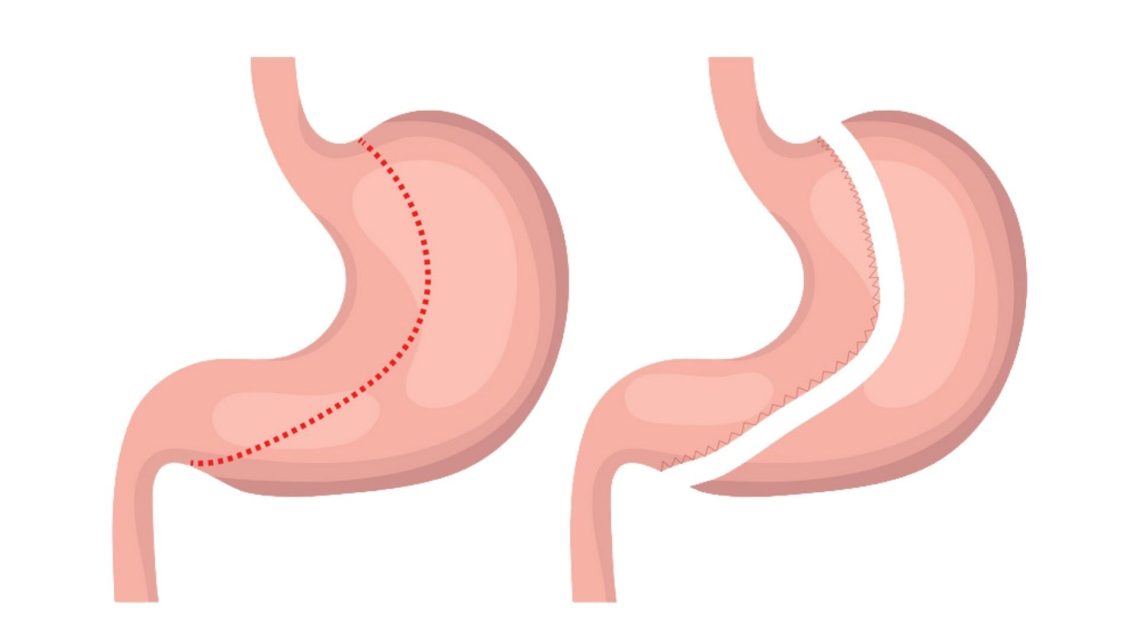
The origins of the gastric sleeve procedure can be traced back to the 1980s when it was initially conceived as the first stage of a more complex surgery known as the duodenal switch. Surgeons observed that removing a portion of the stomach led to substantial weight loss by restricting food intake and altering gut hormones. This realization laid the groundwork for the development of the standalone gastric sleeve surgery.
Early Innovations and Techniques
In its early iterations, the gastric sleeve procedure was performed using open surgery, which involved large incisions and longer recovery times. However, with advancements in laparoscopic techniques in the 1990s, surgeons began to perform the procedure using minimally invasive methods. This shift significantly reduced surgical trauma, postoperative pain, and recovery periods, making the surgery more accessible to a wider range of patients.
As the technique evolved, surgeons refined their approach to achieve optimal outcomes while minimizing complications. Innovations such as the introduction of staple line reinforcement and precise calibration of the sleeve size contributed to improved safety and efficacy. These refinements helped mitigate concerns related to staple line leaks and postoperative complications, enhancing the overall reliability of the procedure.
The Rise of Robotic Surgery
In recent years, the advent of robotic-assisted surgery has revolutionized the field of bariatric surgery, including gastric sleeve procedures. Robotic platforms offer surgeons enhanced visualization, dexterity, and precision, allowing for more intricate maneuvers in confined spaces. This technology has enabled surgeons to perform gastric sleeve surgeries with greater accuracy and reproducibility, leading to improved patient outcomes and shorter hospital stays.
The integration of advanced imaging modalities, such as intraoperative fluoroscopy and indocyanine green angiography, has further refined surgical techniques by providing real-time feedback and ensuring optimal tissue perfusion during the procedure. These technological innovations represent a significant leap forward in the evolution of gastric sleeve surgery, ushering in an era of unprecedented precision and safety.
Personalized Approaches and Tailored Solutions
As our understanding of obesity and metabolic health continues to evolve, so too does the approach to bariatric surgery. Modern techniques emphasize a personalized approach, taking into account individual patient characteristics, metabolic profiles, and lifestyle factors. Surgeons now tailor the size and shape of the gastric sleeve to meet the unique needs and preferences of each patient, ensuring optimal weight loss and metabolic outcomes.
Furthermore, the integration of multidisciplinary care models, including nutrition counseling, behavioral therapy, and postoperative support, has become standard practice in many bariatric programs. This holistic approach addresses the complex interplay between biological, psychological, and social factors underlying obesity, thereby maximizing the long-term success of gastric sleeve surgery.
Looking Ahead: The Future of Gastric Sleeve Surgery
As we look to the future, the evolution of gastric sleeve surgery shows no signs of slowing down. Ongoing research efforts aim to further optimize surgical techniques, enhance patient selection criteria, and refine postoperative management strategies. The emergence of novel technologies, such as endoscopic suturing systems and intragastric balloons, promises to expand the treatment armamentarium and offer new options for patients who may not be candidates for traditional surgery.
Moreover, advancements in our understanding of obesity-related pathophysiology, including the role of gut microbiota and neurohormonal regulation, hold the potential to unlock new therapeutic targets and personalized interventions. By embracing a comprehensive approach that integrates medical, surgical, and lifestyle interventions, we can continue to push the boundaries of what is possible in the treatment of obesity and metabolic disease.